Case contribution: Dr Radhiana Hassan
Clinical:
- A 76 years old man
- Under medical team for investigation of incidental findings of lung mass
- Referred from medical to surgical team for acute abdomen
- Sudden onset of severe abdominal pain immediately after US-guided biopsy of right renal pelvic mass
- First attempt with 16G needle obtained good tissue
- Second attempt aspirated greenish bile material
- Clinically abdomen not distended but guarded, tenderness at puncture site at right subcostal axillary line region
- HB: 14, TWBC: 20, Plt 589

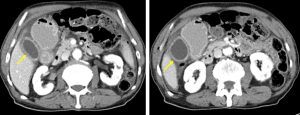
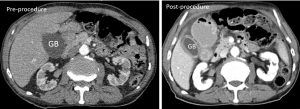
CT scan findings:
- The gallbladder is well distended, located near the right anterior abdominal wall (yellow arrows) which is adjacent to the possible puncture site (as evident by subcutaneous air).
- The gallbladder wall is thickened and enhanced with associated pericholecystic fluid. These changes are not seen in the previous study.
- there is no apparent irregularity of the gallbladder wall or focal area of wall discontinuation observed.
- There is also minimal free fluid seen (mean HU 11) at perihepatic and sub hepatic which tracking into the right paracolic gutter and accumulating within the pelvis.
Intra-operative findings:
- Exploratory laparotomy done
- Upon entering the peritoneum bile coloured peritoneal fluid seen
- Small bowel mildly dilated
- Noted small perforation at the right lateral gallbladder, size of perforation about 1mm
- Oozing of bile from the site of perforation
Diagnosis: Iatrogenic gallbladder perforation.
Discussion:
- Gallbladder perforation is an uncommon complication of percutaneous biopsy
- Conservative management for a short time is appropriate but early sign of peritoneal irritation demand surgical intervention
- There is no specific set of findings which are of diagnostic of gallbladder injury.
- Ultrasound may reveal heterogeneous hyperechoic blood adjacent to the gallbladder, as well as pericholecystic fluid.
- CT is more accurate for identifying blood or discontinuity of the gallbladder wall
- In the setting of bile peritonitis, preoperative imaging should not delay return to the OR for evaluation due to risk of sepsis and shock.
