Case contribution: Dr Radhiana Hassan
Clinical:
- A 44 years old lady
- No known medical illness
- Presented with right sided abdominal pain
- Colicky in nature
- No fever, no vomiting, no altered bowel habit
- Physical examination is unremarkable
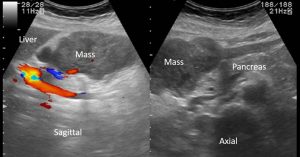

Ultrasound findings:
- Two soft tissue lesions are seen.
- One lesion located inferomedial to the liver and
- another one is in the right iliac fossa region.
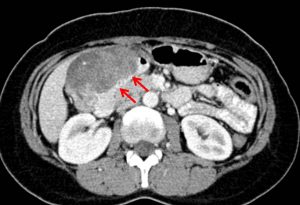


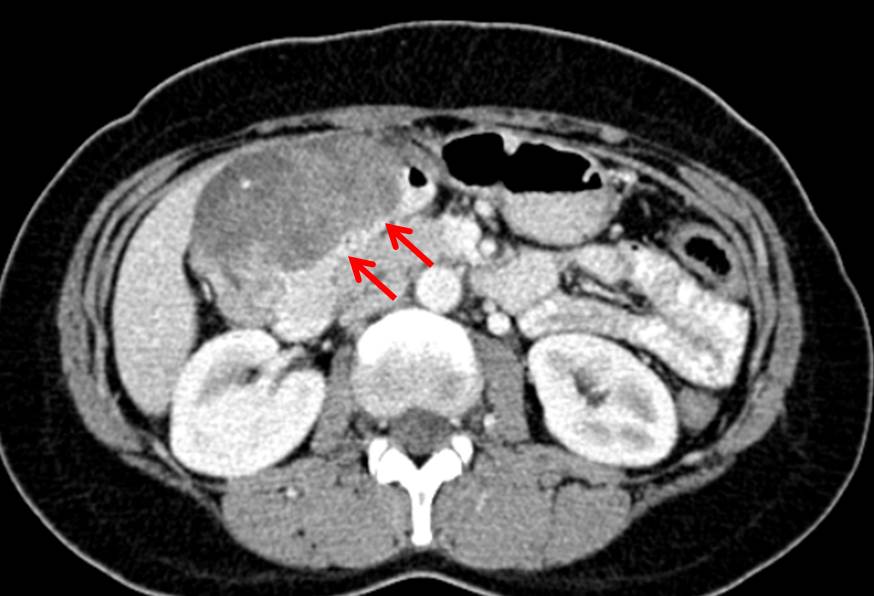
CT scan findings:
- Ct scan abdomen and pelvis shows large soft tissue mass with heterogenous enhancement most probably arising from anterior wall of distal stomach or D1 of duodenum causing luminal narrowing of duodenum (red arrows).
- Another lesion is seen at right iliac fossa region (white arrow).
- A small hypodense is also seen in Segment VI of the liver (blue arrow).
Histopathological findings:
- Macroscopy: Biopsy from D1 consist of a piece of whitish tissue measuring 3x2x3 mm. Submitted in one block.
- Microscopy: serial levels show two fragments of small intestinal tissue covered with villiform epithelium. An occasional goblet cells are noted. Underneath is the small lesional area displaying proliferation of ovoid to spindle cells. An occasional mitosis is identified. The stroma is myxoid in areas. No area of necrosis seen. This lesional area is positive of CD117 antibody
- Interpretation: Duodenum mesenchymal tumours suggestive of Gastrointestinal Stromal Tumour (GIST).
Final diagnosis: Malignant GIST of small bowels
Discussion:
- Gastrointestinal stromal tumours are the most common mesenchymal tumour of the GI tract.
- Usually occur after 40 years of age, most seen in older patients
- Equal in male and female incidence
- Stomach is the most common site
- Clinical presentation depends on location and size of tumour
- Location: stomach (70%), small intestine (20-25%), anorectum (7%), colon and esophagus (uncommon)
- Extra-GIT are known to occur in mesentery, omentum and retroperitoneum. Metastatic lesion may also seen in malignant extra-GIT GIST
- On CT scan, seen as soft tissue mass with central necrosis, calcification is uncommon (3%), typically peripheral enhancement, LN enlargement is not a feature
- MRI depends on presence of necrosis, hemorrhage and cystic changes
Progress of patient:
- OGDS : external compression near antrum and proximal D1, smooth lumen, no obvious mucosal lesion, able to enter D2
- Colonoscopy normal
- Operated done: segmental resection of duodenal GIST + distal gastrectomy + Roux-en-Y gastrojejunostomy + jejunojejunostomy
- HPE: malignant GIST
- Referred to oncology for chemotherapy
- Patient defaulted follow up
- Presented again 5 months after the operation with abdominal pain and vomiting

Repeat CT scan show multiple liver lesions with lymphadenopathies and right pleural effusion. Patient opted for conservative management.
Recent Comments