Clinical:
- A 3 years old boy
- Under follow up at another hospital for left parotid swelling for one year
- Claimed that ultrasound done showed cystic lesion, planned for CT scan on next visit
- Presented with sudden increase in size of swelling at left parotid
- Currently painful and associated with fever and trismus
- Clinically a huge swelling at left parotid
- Soft, tender, erythematous, fluctuant and no punctum
- Unable to properly examine the oral cavity due to trismus
- No facial asymmetry
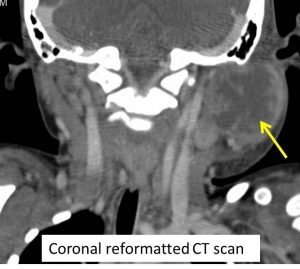
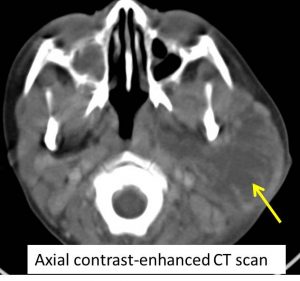
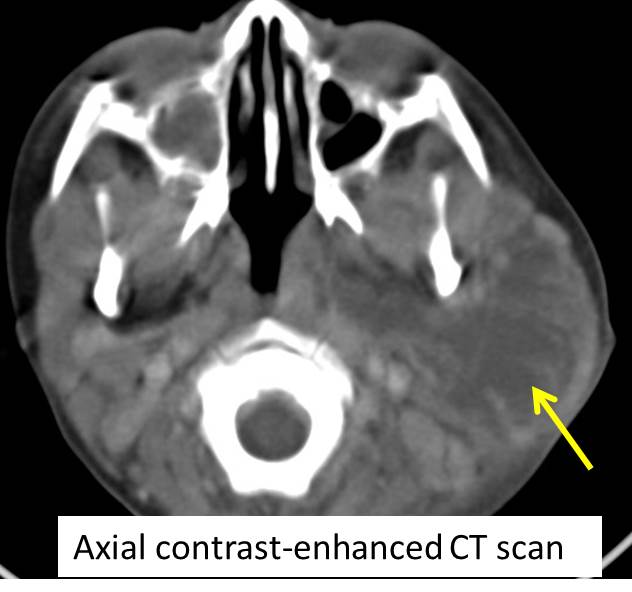
CT scan findings:
- Left parotid gland is enlarged and predominantly cystic with thick and irregular enhancing wall. There are septae within the lesions which also enhances post contrast.
- There is no calcification or fluid levels within the lesion.
- Anteriorly it extends to the left facial region causing minimal mass effect to the posterior part of left masseter. However the masseter muscle is normal.
- Posterolaterally it also compressed and displaced the sternocleidomastoid muscle. Similarly, no obvious abnormality is seen within this muscle.
- Medially there is extension of the lesion with involvement of the deep parotid lobe and occupies the left parapharyngeal space.
- The ICA and IJV are patent.
- The overlying fat planes are streaky, however no obvious thickening of the skin seen.
- There are multiple enlarged nodes at the submandibular and also along the jugular chains superior and inferiorly.
- There is no lytic lesion of the adjacent bone.
- No extension into retrosternal or upper thoracic cavity
- Impression: Features are suggestive of left parotid abscess.
Intra-operative findings:
- Incision and drainage done
- Cystic mass 10×10 cm, soft, fluctuant, no punctum
- 40 cc straw coloured pus drained upon entering sac
- Cavity wash with povidone
HPE findings:
- Macroscopy: specimen labelled as cyst wall, consist of multiple pieces of brownish tissues
- Microscopy: Section shows fragments of tissue composed of neutrophils collection forming abscesses. Areas of necrosis and haemorrhage are noted. No viable parotid tissue included
- Special stain for Zeihl-Neelson to look for AFB and PAS for fungal bodies are negative
- Interpretation: consistent with abscess wall
Diagnosis: Left parotid abscess
Discussion:
- An infection of the parotid gland can arise from ascending infection via Stensen’s duct, or from bacteraemia or viremia.
- It can lead to suppurative changes, which can result in abscess formation. If the process continues pus penetrates the capsule and invades the surrounding tissue, and extends downward into the deep fascial planes of the neck, backward into the external auditory canal, or outward into the facial skin
- The predisposing conditions and precipitating factors include: dehydration, poor oral hygiene, dental infection, oral trauma, xerostomia, ductal obstruction, certain drugs (anticholinergics and antihistamines), certain chronic diseases (Sjogren’s syndrome and diabetes mellitus), malnutrition, pre-existing parotid Warthin’s tumor, immuno-suppression and sialolithiasis
- Ultrasonography is the method most frequently used for assesment, for its non-invasiveness, the wide distribution, rapid and easy to perform and the low cost. It allows a detailed morphological evaluation of the gland and has an important value, complementary to clinical examination, in the study of parotid inflammatory diseases, defining the characteristics of the lesion and, in a large number of cases, also its nature.
- However in complicated cases or very large lesion, CT scan is helpful in preoperative assessment to review the extension of lesion.
Progress of patient:
- Patient was discharged well 3 days after operation
- Last review one month later was uneventful.
Recent Comments