Clinical:
- A 57 years old lady
- Underlying HPT and bronchial asthma
- Treated as CVA since 3 years ago when presented with right upper limb weakness and numbness
- CT scan brain shows no obvious infarction
- Complaint of worsening right upper limb weakness and numbness at bilateral fingers
- Clinical examination shows GCS 15/15. Power C1-C3: 5/5, C4-C7: right 4/5 and left 5/5 and C8: right 4/5 and left 5/5
- Tone increased on right UL, hyperreflexia right UL and LL
- Babinsky downgoing
- MRI brain was performed to evaluate lacunar infarctions showed normal findings
- Abnormality noted at cervical spine region and MRI cervical spine done on the same day

MRI findings:
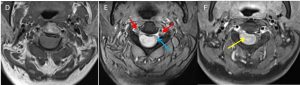
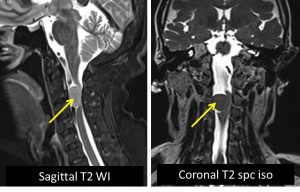
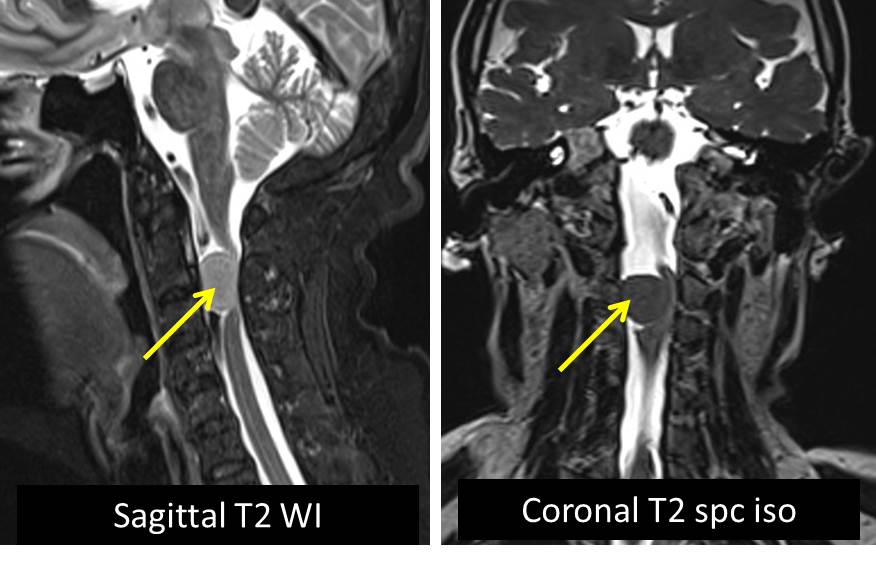
- There is a right sided oval-shaped intra-dural extra-medullary mass (yellow arrows) located at the C2/3 junction region. It measures at about 1.0 x 1.9 x 1.9cm.
- It returns hypointense signal on T1, subtly hyperintense relative to the cord on T2, hyperintense on T2 TIRM and enhances post contrast.
- It can be seen displacing the cord to the left, with marked effacement of the cord seen (blue arrow). No significant myelopathic changes observed.
- The right sided exiting nerve root can be seen within the exit foramen, but the portion of the nerve root within the spinal canal is likely impinged by the mass.
- No extension of the mass into the exit foramen noted. No widening of the adjacent exit foramen observed (red arrows).
- The surrounding bony structures are normal.
- Impression: Intra-dural extra-medullary cervical mass. MR features are most probably indicative of a spinal meningioma.
HPE findings:
- Specimen labelled as cervical C2/C3 tumour consists of multiple pieces of whitish tissue measuring 27 mm in aggregate diameter.
- Microscopy: sections show fragments of tumour tissues composed of lobules of tumour cells. The tumour displays a generally uniform oval nucleus with central clearing and indistinct cytoplasmic borders. In areas, multiple tight whorls of tumour cells are also present. Mitosis is occasionally seen (3 per 10HPF). There are several psammoma bodies noted. There are also multiple intervening hyalinized vessels present within the tumour tissue. No necrosis noted.
- Immunohistochemical studies show: EMA positive, Vimentin positive, S100 negative and GFAP (glial fibrillary acidic protein) negative.
- Interpretation: Meningothelial meningioma, WHO grade 1
Diagnosis: Spinal meningioma
Discussion:
- Spinal meningiomas represent a minority of all meningiomas (approximately 12%).
- They have a peak incidence in the 6th to 8th decades
- Spinal meningiomas have a strong sex predilection in adults, stronger than that seen with intracranial meningiomas, with females accounting for 75-90% of cases.
- In children, there does not appear to be a sex predilection
- Most meningiomas are solitary lesions (98%). Multiple meningiomas are most often associated with Neurofibromatosis 2.
- The vast majority (90%) of spinal meningiomas are intradural extramedullary in location. Occasionally (5%), purely extradural tumors are found. The remainder (5%) have both intradural and extradural components taking on a dumb-bell appearance.
- Spinal meningiomas are not distributed evenly along the canal:
- cervical spine: 15%
- thoracic spine: 80%
- lumbosacral spine: 5%
- Most spinal meningiomas are benign, with 70-90% being classified as WHO Grade 1 lesions
- The most common spinal meningioma histology is WHO grade I meningothelial meningioma (80%)
- This case illustrates the commonest form of spinal meningioma and its typical imaging characteristics.
Progress of patient:
- Operation done to remove the tumour
- Review one month after operation showed improvement of upper limb and lower limb power
- Patient is able to move neck
Recent Comments