Clinical:
- A 53-year old lady
- Underlying history of chronic rheumatic heart disease, hypertension and hyperlipidaemia
- Presented with acute onset of left sided hemiparesis.
- GCS score was 15/15.
- Urgent plain CT brain was performed and repeated after three days due to worsening of clinical condition.
CT scan findings:
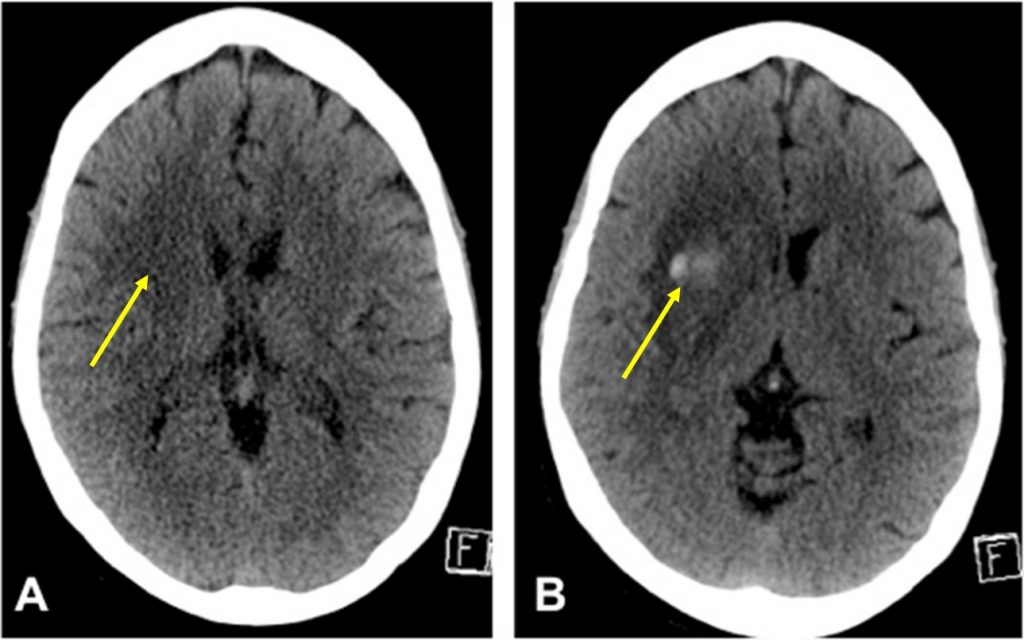
- The first non-contrast axial CT brain (A) shows a subtle hypodensity in the right frontal region. Minimal compression effect to ipsilateral lateral ventricle and effacemen of adjacent cerebral sulci also seen.
- Subsequent CT scan a few days later shows more pronounced hypodense area with new hyperdensities within it. There is worsening of compression effect to ipsilateral lateral ventricle. No midline shift.
Diagnosis: Haemorrhagic transformation of cerebral infarction.
Discussion:
- Hemorrhagic transformation of an ischaemic infarction is one of the complications of cerebral infarction and can significantly worsen prognosis.
- The rates of hemorrhagic transformation after ischemic strokes have been variably reported.
- Generally over half of all cerebral infarctions at some stage develop hemorrhagic component but majority (89%) are petechial hemorrhages and a small percentage (11%) had hematomas.
- Cardioembolic strokes are more likely to undergo hemorrhagic transformation than atherothrombotic strokes.
- Hemorrhagic transformation can occur spontaneously at an overall rate of 5% (hematomas). However, it is more frequent in patients who receive anticoagulant therapy and even more frequent in those undergoing thrombolytic therapy.
