Clinical:
- A 61 years old Malay female
- Presented with bilateral lower limb weakness
- Posterior instrumentation for compression fracture of T4 done
- HPE from bone negative for malignancy
- Noted to have neck swelling. No symptoms related to the neck mass.
- Thyroid function test was normal


Radiographic findings:
- Soft tissue mass at right side of the neck
- The mass is displacing the trachea to the left side (white arrows)
- No obvious luminal narrowing of the trachea is seen
- There is calcification noted within the soft tissue mass (yellow arrows)

Ultrasound findings:
- Multiple nodules of varying sizes which are predominantly solid, well-defined and heterogenous are seen occupying the right thyroid lobe.
- The largest nodule seen measures at 3.0 x 2.7 cm.
- Specks of calcification is noted within the lesion (yellow arrow).
- Otherwise both CCA and IJV are patent.
- A few nodes also seen (images not shown)
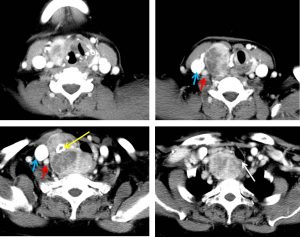
CT scan findings:
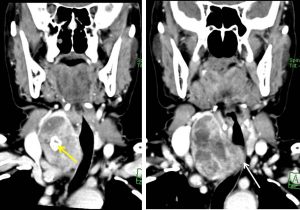
- Grossly enlarged right thyroid lobe, measuring about 5.6 (W) x 5.4 (AP) x 6.8 cm(length) with retrosternal extension.
- It is heterogeneously enhanced with multiple areas of non-enhancing and minimally enhanced lesions within.
- Coarse calcification is also noted within (yellow arrow).
- The mass causes compression and displaced the larynx and upper trachea to the left side (white arrow).
- Significant compression is seen extending from C7/T1 till the sternal notch (about 1.7 cm in length). The narrowest lumen of the trachea is at the level of T1, about 4.0 cm below the glottis which measures approximately 1.6 (AP) x 0.7 cm(width).
- There are multiple cervical, submandibular and submental nodes seen bilaterally. The largest node measures 1.0 x 1.6 cm at the right jugular region.
- The internal jugular veins and both carotid arteries are normal (blue and red arrows respectively).
HPE findings:
- Macroscopy: specimen labelled as total thyroidectomy. Grossly asymmetrical enlarged right thyroid lobe. The outer surface is smooth with no capsular breach seen. Cut section of right thyroid lobe shows a firm whitish lesion measuring 7x5x22 mm at the midpole. The rest of the thyroid lobe shows multinodular lesion ranging from 25 to 55 mm at the middple pole. The nodules has greyish to brownish surface with areas of hemorrhage and calcification noted.
- Microscopy: Sections from the thyroid lobe shows a multiple foci of malignant cells arranged in papillary structures with some in follicular and trabecular pattern. The tumour cells display an enlarged nuclei, oval to round optically clear nuclei, irregular nuclear contour with nuclear grooving. Occasional nuclear pseudo-inclusions are seen. Scattered mitosis are noted. In areas, calcification and infarcted thyroid follicles are identified. The nearest distance between tumour cells and left thyroid capsule is 4 mm. No capsular breach seen.
Diagnosis: Papillary thyroid carcinoma.
Discussion:
- It is the most common thyroid carcinoma comprising about 88% of all thyroid carcinomas.
- It usually occurs in middle age groups; peak at 4th to 5th decade
- It is more common in female.
- Papillary carcinoma has a tendency to metastasize early to local lymph nodes, with 50% of patients having nodal involvement at presentation.
- Distal haematogeneous dissemination is less common with a prevalence of only in 5-10% of patients at presentation.
- Ultrasound usually appears as a solitary mass usually with an irregular outline, located in the subcapsular region and demonstrating vascularity . These features are not seen in this case.
- Small punctate regions of echogenicity representing microcalcifications may be present. In this case it showed intralesional coarse calcification.
Progress of patient:
- Total thyroidectomy done.
- Radioactive iodine treatment
- Patient develop progressive worsening of lower limb weakness and became paraplegia
- MRI showed multiple vertebral metastasis
- Condition complicated with sepsis secondary to infected sacral sore and pneumonia
- Patient passed away 5 months after diagnosis

Recent Comments