Case contribution: Dr Radhiana Hassan
Clinical:
- A 69 years old man
- No known medical illness
- Presented with lateral tongue swelling for 6 months
- Gradually increase in size
- Associated with loss of appetite and loss of weight
- Had multiple episodes of spontaneous bleed from the lesion
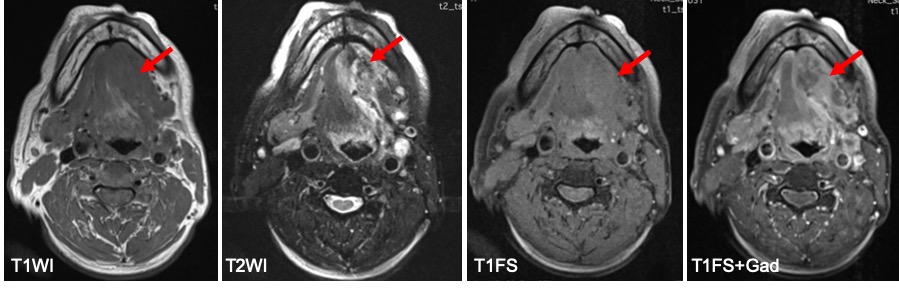
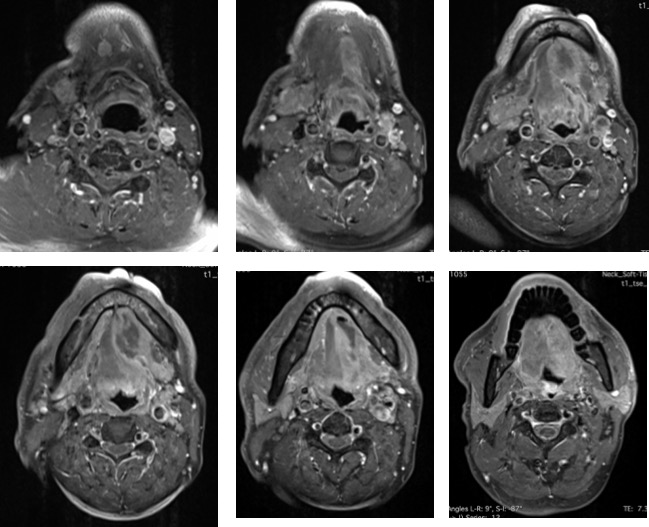
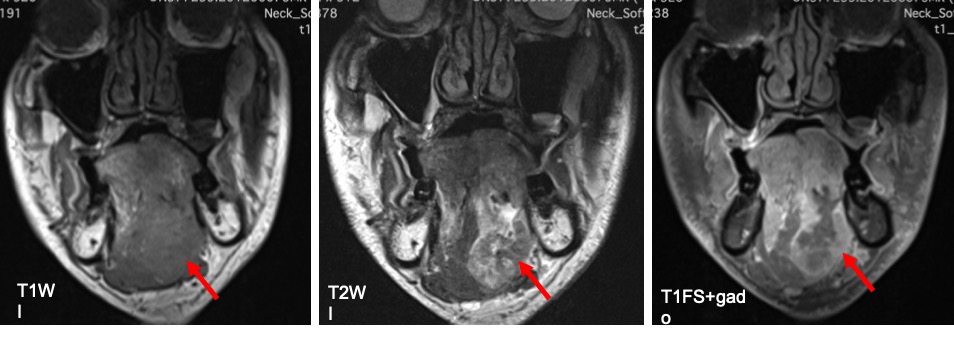
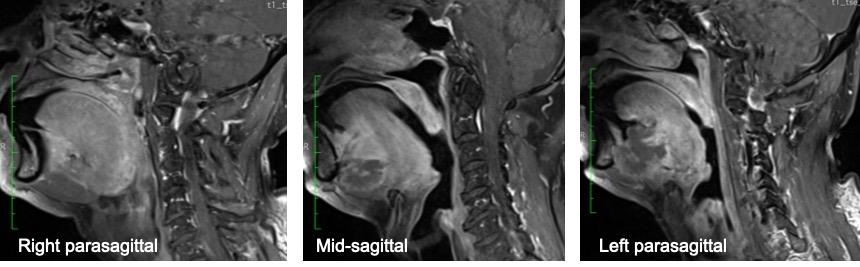
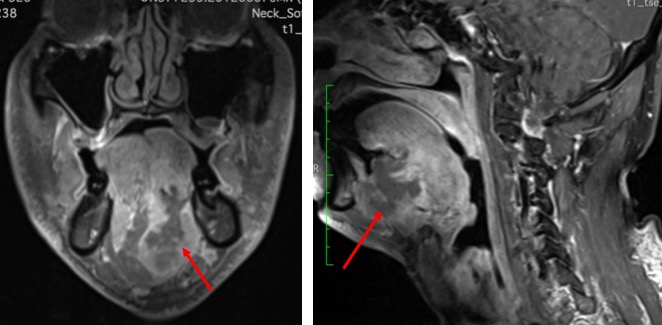
MRI findings:
- A huge mass is seen at left sublingual region
- The lesion extends and involve the root of tongue, base of tongue and cross the midline.
- The lesion is isointense to muscle on T1, heterogeneously hyperintense on T2 and shows heterogenous marked enhancement post contrast. Central part of lesion less enhanced.
- The lesion extends and cross midline with involvement of genioglossus, styloglossus, geniohyoid and mylohyoid muscles
- A few enlarged nodes are also seen at Level II and Level III
HPE findings: Adenoid cystic carcinoma
Discussion:
- It is a rare malignant neoplasm that accounts for 1–2% of all head and neck malignancies and approximately 10% of all salivary gland tumours.
- The most frequent site is parotid gland (30%) followed by submandibular region and minor salivary glands.
- The reported frequency in tongue is 19.8% with 85% observed at base of tongue.
- It is characterized by slow, indolent growth and late metastases.
- Local recurrence of ACC is common despite aggressive surgical resection due to extensive local tissue infiltration and perineural spread.
- The lungs are the most common site of distant metastases. Other sites include brain, bone, liver, thyroid, and spleen.
- Overall adenoid cystic carcinoma caries a grave prognosis, survival rate 58% at 5 years and declined to 16% at 15 years.
- On CT or MRI, adenoid cystic carcinoma cannot be distinguished from SCC or other malignancies.
- T2-hyperintense signal correspond to low cellularity tumour and associated with good prognosis.
- Perineural spread is common. On CT perineural spread is seen as enlargement of skull base foramina and fissures such as foramen ovale (V3), foramen rotundum (V2) and pterygopalatine fissure (V2). On MRI it may demonstrate increased thickness of the affected nerve and diffuse or marginal enhancement post contrast.
Recent Comments