Case contribution: Dr Radhiana Hassan
Clinical:
- A 23-year old who was involved in MVA with altered sensorium.
- A serial plain CT brain was performed.
Imaging findings:
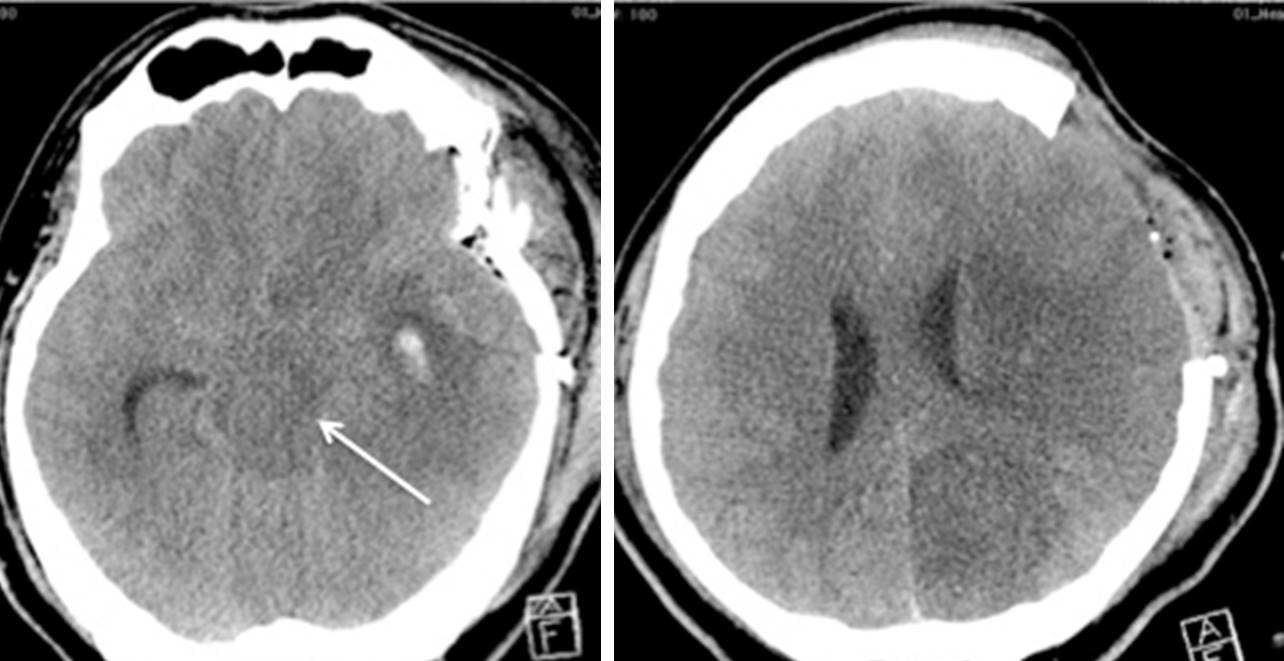
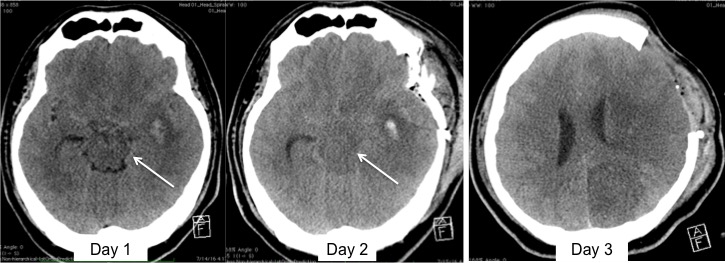
- CT brain showed intra-parenchymal hemorrhage in the left temporal region with minimal perilesional oedema.
- The changes caused compression of the ipsilateral ambient cistern (arrow).
- Repeat CT scan after one day showed worsening of his condition.
- Presence of descending transtentorial herniation on the left side was seen with obliteration of the basal cistern more on the left side.
- This internal brain herniation possibly caused compression of the left MCA and PCA causing cerebral infarction one day later. Note the vascular territorial hypodensity seen on the last scan.
- Craniectomy was done to release the intracranial pressure.
Diagnosis: Post-traumatic cerebral infarction.
Discussion:
- Post-traumatic cerebral infarction is one of the most severe secondary effect after traumatic brain injury.
- It is associated with poor outcome and high mortality rate.
- The incidence of post-traumatic cerebral infarction was reported ranging from 2% to 10%.
- Various mechanism have been suggested for this complication including direct vascular compression by mass effect as in this case by the internal brain herniation, dissection, embolization, cerebral vasospasm and systemic hypoperfusion.
- It is postulated that PCA infarction occurs as the vessel is compressed against the rigid edge of the tentorium by the herniating mass of the medial temporal lobe producing posterior cerebral infarction.
- Similar pressure effect was postulated for MCA infarction with other contributing factors including stretching and attenuation of the vessel by increased intracerebral pressure and cerebral oedema.