Case contribution: Dr Radhiana Hassan
Clinical:
- A 19 years old female
- History of epilepsy since childhood
- Recently diagnosed glaucoma
- No abnormal cutaneous sign
- Complaint of headache
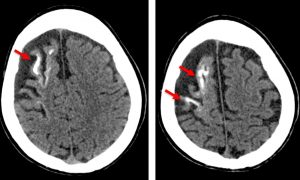
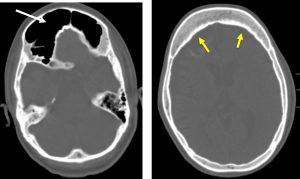
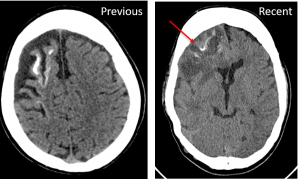
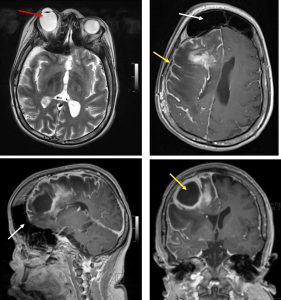
CT scan findings:
- Volume reduction involving the right frontal, temporal and parietal lobes with adjacent prominent sulci in keeping with brain atrophy.
- There is ‘tram track ‘ gyriform calcification at the right frontal lobe (red arrows).
- There is thickening of the adjacent skull vault (white arrow)
- Enlargement of the frontal sinuses is also seen (yellow arrows).
- No other lesion at the rest of brain parenchyma. No hydrocephalus.
Diagnosis: Sturge-Weber syndrome
Discussion:
- Sturge-Weber syndrome is a rare syndrome
- It is also known as encephalotrigeminal angiomatosis
- The diagnosis is usually obvious with congenital facial cutaneous known as port wine stain or facial nevus flammeus
- In 5% of cases, there is intracranial involvement without associated cutaneous nevus
- In the majority of cases the nevus is unilateral and ipsilateral to the intracranial abnormality
- The commonest presentation is childhood seizure , often associated with developmental delay and hemmispheric symptoms including hemiplegia /hemiparesis
- Approximately a third of patients have choroidal or scleral angiomatous involvement which may be complicated with retinal detachment, buphthalmous or glaucoma
- Skull x-rays:
- historically used to identify gyriform calcification.
- Findings are usually evident between 2 and 7 years of age
- historically used to identify gyriform calcification.
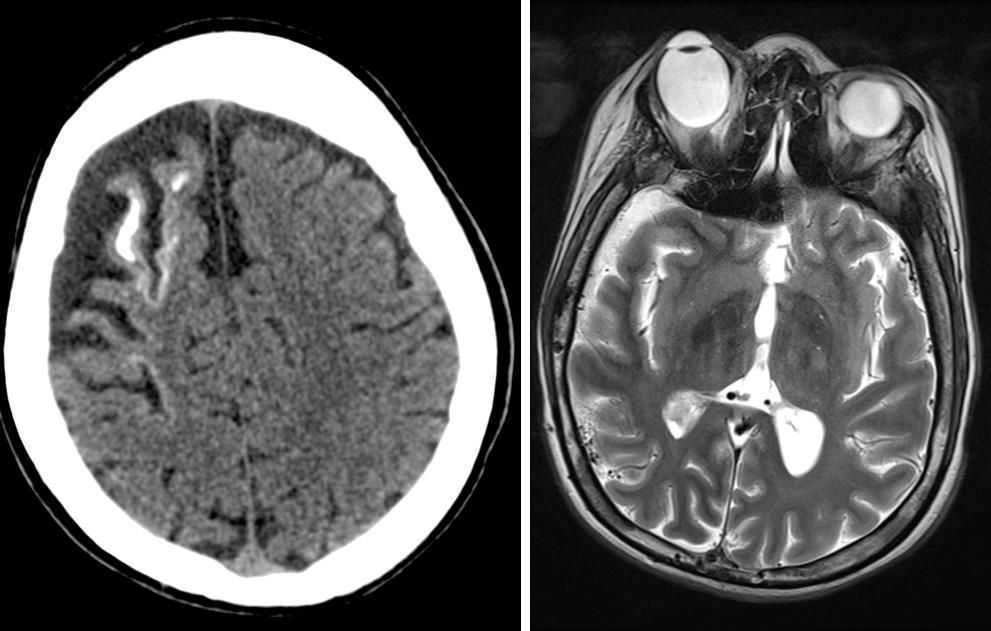
- CT scan:
- subcortical calcification and associated parenchymal volume loss,
- calvarial and regional sinus enlargement,
- ispilateral choroid plexus enlargement,
- asymmetric cavernous sinus enlargement,
- orbital choroidal hemangiomas
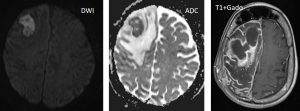
- MRI:
- T1WI shows volume loss,
- T1+Gado shows prominent leptomeningeal enhancement in the affected area due to congested internal veins resulting in venous congestive ischaemia. But later in life, the angioma may be losing enhancement. Dilatation of transparenchymal veins that communicates between superficial and deep venous systems.
- T2WI shows low signal in white matter subjacent to angioma,
- SWI/GE shows blooming artifact from the calcifications,
- MRS shows decreased NAA
- Angiography (DSA) is abnormal in most of cases (80%) and demonstrate absent superficial cortical veins with abnormal and enlarged deep venous drainage
Progress of patient:
- Presented again 3 years later with right frontal abscess